According to the 2022 “State of Lung Cancer” report (1), someone is diagnosed with lung cancer every 2 ½ minutes, and 356 lung cancer patients die every day. Lung cancer has one the lowest 5 year survival rates – 25% – despite significant improvement in treatments. This is in great part due to late stage diagnosis. Forty-four percent of cases are diagnosed at a late stage, where survival is only 7%. And only 5.8% of high risk individuals are screened.
If you are thinking about starting or have already started a lung cancer screening (LCS) program, that should be applauded. The goal is to diagnose lung cancer while it’s still potentially curable. So screening high risk patients – to find nodules that may be cancerous or evolve into lung cancer – makes perfect sense.
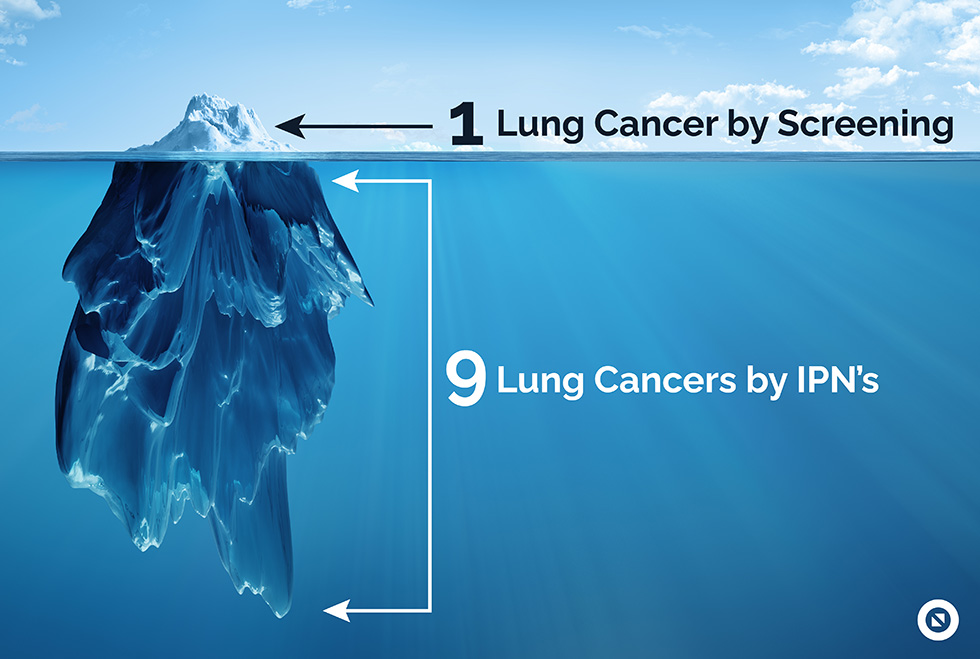
But screening high risk populations to find lung cancer is only finding the tip of the iceberg. Submerged below – and commonly missed until it’s too late – are incidental pulmonary nodules (IPNs) that become lung cancer. IPNs are just as important – and deadly – and 9 times more common than pulmonary nodules/cancers found by screening (2).
Less than 10% of health systems have some type of IPN program (3). If you do NOT have a well designed and implemented IPN program to complement your LCS program, you are missing a lot of lung cancer (and are likely not even aware).
- over a 3rd of chest CTs will have an IPN (4)
- the rate of malignancy for IPNs overall is about 5% (similar to the malignancy rate in lung cancer screening) (5,6)
- follow-up IPN care fails in about 70% of cases (7).
What does that mean in very practical terms? It means that for every 90 chest CT scans you read (as a radiologist) or order (as a provider), one lung cancer will be missed. For an average hospital that performs about 2,000 chest CTs a year, that translates into about 22 lung cancers missed, or at the very least a significant delay in care- potentially missing the opportunity to provide curative intent therapy. Realizing a true system-wide stage shift in lung cancer demands that IPNs are captured and managed appropriately.
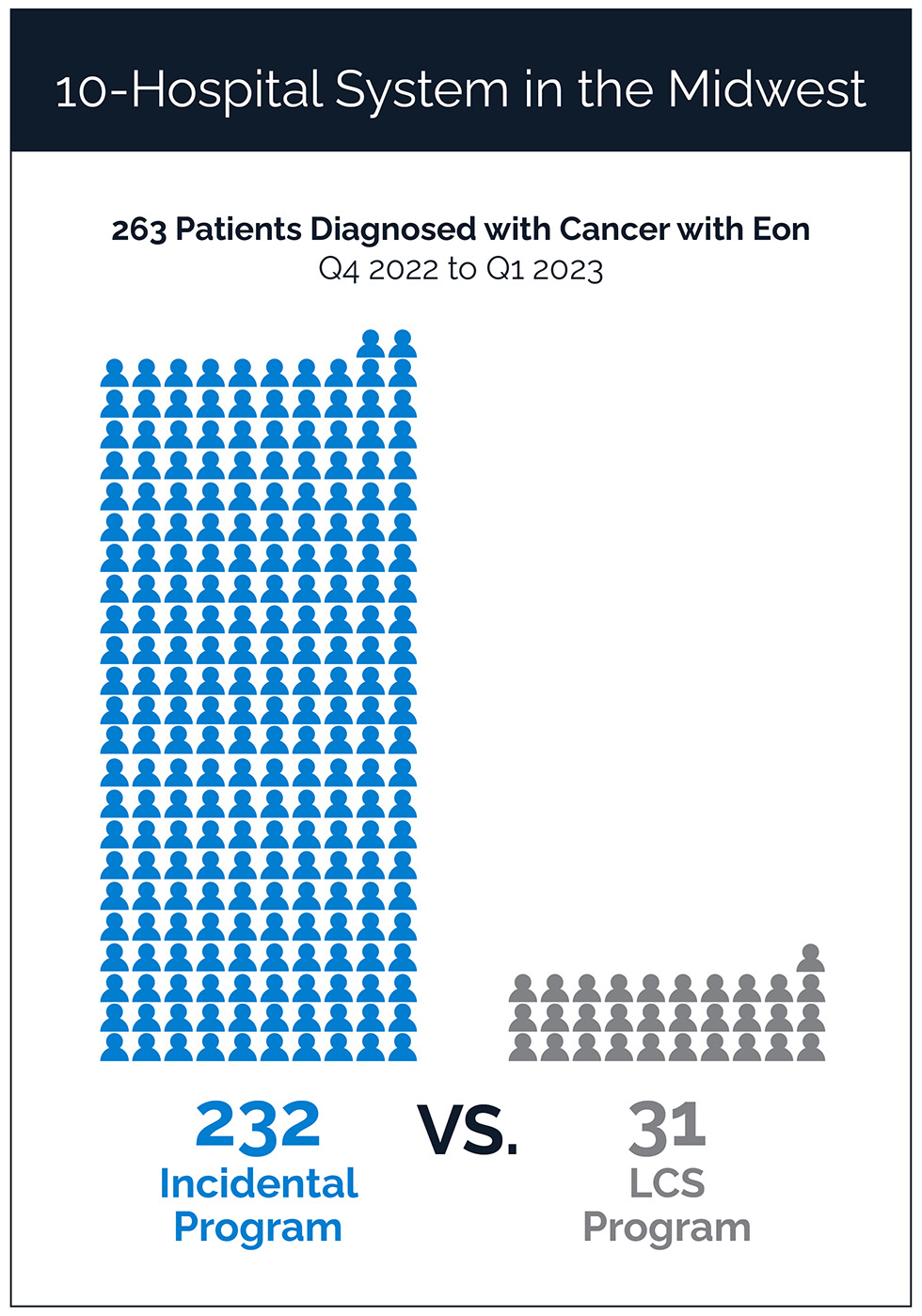
If you IMPLEMENT a well-designed incidental lung program, you will find 7-8 times as many lung nodules AND lung cancers as you will find with your LCS program (8).
Well-developed IPN programs are showing improvements in both clinical processes and outcomes – diagnosing patients with earlier (curable) stage lung cancer (9-12) and retaining patients in their network for the care they need.
And there you have it.
- Incidentally found pulmonary nodules and cancers are 9 times more common than those found through lung cancer screening programs.
- Without a well-designed and implemented IPN program, about 70% of nodules are missed, and 5% of those missed nodules are or will become cancer.
- Comprehensive Lung Programs that include tracking and management of IPNs alongside Lung Cancer Screening can lead to stage shift and generate significant downstream revenue
- And there are many other cancers that start as incidental findings that need reliable follow-up as well – thyroid, pancreas, liver, and breast to name a few.
How do I get started?
Innovative organizations realize the importance of comprehensively managing both screening and incidental pulmonary nodules to catch and treat as many potential cancer patients as possible. But how do I make the internal case for an incidental findings program at my facility? Here’s how to get started:
- Pull together lung cancer incidence data for your area
- Find the right lung coordinator and/or navigator – Seek out a leader who is a master communicator and can train others on processes that will help ensure the long-term success of your program
- Build a multidisciplinary team – Coordinate a multi-faceted team of experts who specialize in different aspects of care and meet regularly in a nodule board to discuss suspicious IPNs
- Seek out the right technology partner – Find a technology partner that can accurately identify abnormalities with few false positives and offers workflow automation to help your team save time
- Understand the downstream impact – Calculate the potential downstream revenue to areas such as pulmonology, interventional pulmonology, thoracic surgery, radiation oncology, medical oncology, and radiology
Interested in understanding the clinical and financial impact of a comprehensive lung cancer screening and incidental program at your facility? Contact us for your custom opportunity assessment.
Click here to learn more about how leading health systems built their lung screening and incidentals program and the results they are seeing.
References:
- State of lung cancer: 2022 report. American Lung Association. November 15, 2022. Accessed November 16, 2022. https://www.lung.org/getmedia/647c433b-4cbc-4be6-9312-2fa9a449d489/solc-2022-print-report
- Osarogiagbon R, Miller E, Faris N, Pinsky P. Incidental pulmonary nodules, lung cancer screening, and lung cancer in the Medicare population. Journal of Clinical Oncology 40, no. 16_suppl (June 01, 2022) 6536-6536. DOI: 10.1200/JCO.2022.40.16_suppl.6536.
- Based on Eon data.
- O’Sullivan J, Muntinga T, Grigg S, Ioannidis J. Prevalence and outcomes of incidental imaging findings: umbrella review. BMJ 2018;361:k2387 http://dx.doi.org/10.1136/bmj.k2387
- Gould MK, Tang T, Liu IL, Lee J, Zheng C, Danforth KN, Kosco AE, Di Fiore JL, Suh DE. Recent Trends in the Identification of Incidental Pulmonary Nodules. Am J Respir Crit Care Med. 2015 Nov 15;192(10):1208-14. doi: 10.1164/rccm.201505-0990OC. PMID: 26214244.
- McWilliams A, Tammemagi M, Mayo J, et al. Probability of Cancer in Pulmonary Nodules Detected on First Screening CT. N Engl J Med 2013; 369:910-919 DOI: 10.1056/NEJMoa1214726
- Lee J, Lisker S, Vittinghoff E, et al. Follow-up of incidental pulmonary nodules and association with mortality in a safety-net cohort. Diagnosis (Berl). 2019 November 26; 6(4): 351–359. doi:10.1515/dx-2019-0008.
- Number of patients who were diagnosed with lung cancer through lung cancer screening or incidental lung program at a 10-hospital system in the Midwest between Q4 2022 to Q1 2023
- LeMense GP, Waller EA, Campbell C, Bowen T. Development and outcomes of a comprehensive multidisciplinary incidental lung nodule and lung cancer screening program. BMC Pulm Med. 2020 Apr 29:20((1)):115
- Roberts TJ, Lennes IT, Hawari S, Sequist LV, Park ER, Willers H, et al. Integrated multidisciplinary management of pulmonary nodules can streamline care and improve adherence to recommendations. Oncologist. 2020 May;25((5)):431–437.
- Van Gerpen R. Creating an incidental pulmonary nodule safety-net program. Chest. 2021 Jun;159((6)):2477–2482.
- Carr L, Dyer D, Zelarney P, Kern E. Improvement in Stage of Lung Cancer Diagnosis With Incidental Pulmonary Nodules Followed With a Patient Tracking System and Computerized Registry. JTO Clin Res Rep 2022 Mar;3(3):100297.

